Background
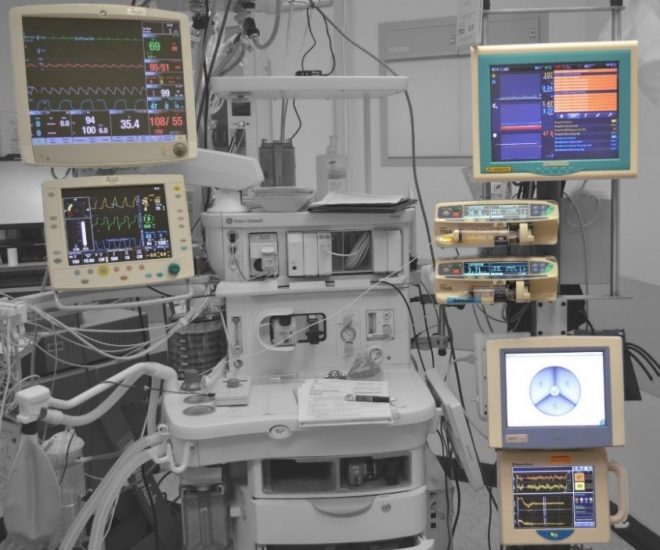
Did you ever wonder in your wildest possible imagination that one day an automated anesthetic machine can sedate a patient without the need for human anesthesiologists? No, right…neither did us! When we first heard about it, it sounded a mere fantasy but to our surprise it is something that scientists are currently working on, in order to make it a reality and a dream come true. We believe just as technology changed automobile factories, this potential automation of drug delivery procedure will one day transform hospitals.
Think of this machine as a sort of humanoid anesthesiologist that thinks like an anesthesiologist, analyses biological information and constantly adapts its own behavior. However, anesthesia is tricky. It’s often compared to flying a plane – keeping a patient hovering in just the right plane of consciousness. Surgeons don’t want patients writhing on the table. And patients don’t want to be aware of the operation. The article discusses the potential, efficacy and feasibility of an automated closed-loop controlled Propofol drug delivery system for clinical surgery.
What is the application?
Anesthesia, a temporary induced loss of sensation or awareness, plays an important role in clinical operations because it allows painless performance of medical procedure that would otherwise cause intolerable pain to an unanesthetized patient. General anesthesia works by altering the flow of sodium molecules into the nerve cells (neurons) through the cell membrane, which then restricts the generation of nerve impulses. The brain becomes unconscious, does not store memories and does not register pain impulses from other areas of the body as a result of the lack of generation of the nerve impulses. Propofol, a commonly administered intravenous general anesthetic agent, is one of the short-acting anesthesia drug that decreases level of consciousness and lack of memory. It is used for starting and maintenance of general anesthesia because the recovery from Propofol is more rapid and clear.
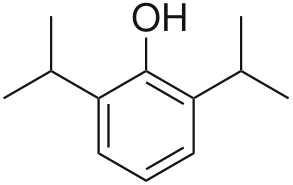
Figure 1. Chemical structure of Propofol
Normally Propofol is administered by an anesthesiologist via an Intravenous line, however a more novel and precise technique- automated closed-loop controlled Propofol delivery system can be used in order to administer the amount of Propofol injection and to control the depth of anesthesia instead of the anesthesiologist manually administering the Propofol intravenous drug which leads to time delay in reading the value and comprehending the change in monitored value as well as human error in reading, judging and altering the drug dosage. Automated anesthesia drug delivery system involves the continuous administration of a combination of drugs with frequent adjustments to maintain normal cardio respiratory vital signs during surgical stimulation. Recent advances in nervous system monitoring technology have yielded a new set of real time sensors to capture the effect of these drugs on the patient’s state. As a result, automated feedback control of anesthetic drug delivery to a pre-defined set point can be a means for providing the patient with a titration specifically adjusted to his or her needs. Moreover, automated closed-loop controlled Propofol delivery system has the potential to decrease drug dosage and facilitate post-operative recovery while increasing patient safety and decreasing the workload of the anesthesiologist.
Why does it need control?
The performance of Propofol drug delivery depends upon the reliability of the controlled variables. While delivering the drug to the patient, there must be some kind of a continuous monitoring system to ensure that the patients are getting the right amount of sedation. The control variables include the measurement of the heart rate, blood pressure, respiration and oxygen level in the blood. The control variables mentioned vary from person to person based upon age, gender, body weight, general health, medical conditions and activity levels. In addition to these direct measures, surrogate measures like Spontaneous and Evoked-Electro-Encephalogram (EEG) should also be considered, which can scan the patient’s brain waves to make sure the sedation is adequate in order to keep the patient in a period of moderate sedation-un aware but still responsive. EEG has been proven to give accurate measure of the drug effect as it assesses the effect of anesthetic drugs on the central nervous system. The delivery of intravenous anesthetic drugs using the apparent relationship between the depth of anesthesia and the changes in EEG increases accuracy. Recently, Bispectral Index (BIS), a derived variable of the EGG that provides a measure of the consistency of phase and power relationships among the various frequencies of EGG, has emerged as a convenient and versatile tool to titrate hypnotic agents and to reduce drug consumption, therefore allowing faster recovery while avoiding side effects such as hemodynamic instability or awareness. BIS is a dimensionless number scaled from 100 to 0, with 100 representing an awake electroencephalogram and 0 representing electrical silence. It describes the complex EGG pattern as a single variable. It was initially calculated to give the best correlation with the probability of movement to surgical incision but then it has been further developed using a database of EGG data collected with different anesthetic drugs. Because it is a single composite measure monitored continuously and reported to be related to the hypnotic component of the anesthetic state superior to other measures, it has been used to control depth of hypnosis automatically.
Unsedated individuals typically have BIS greater than 97. With progressive drug-induced sedation, BIS number declines. During surgery, the appropriate time to start an operation has the signal of stable hemodynamics and no movement or response. The BIS value is determined experimentally, which should be less than 60 but greater than 45. This allows reduced anesthetic dosing, emergence and recovery times.
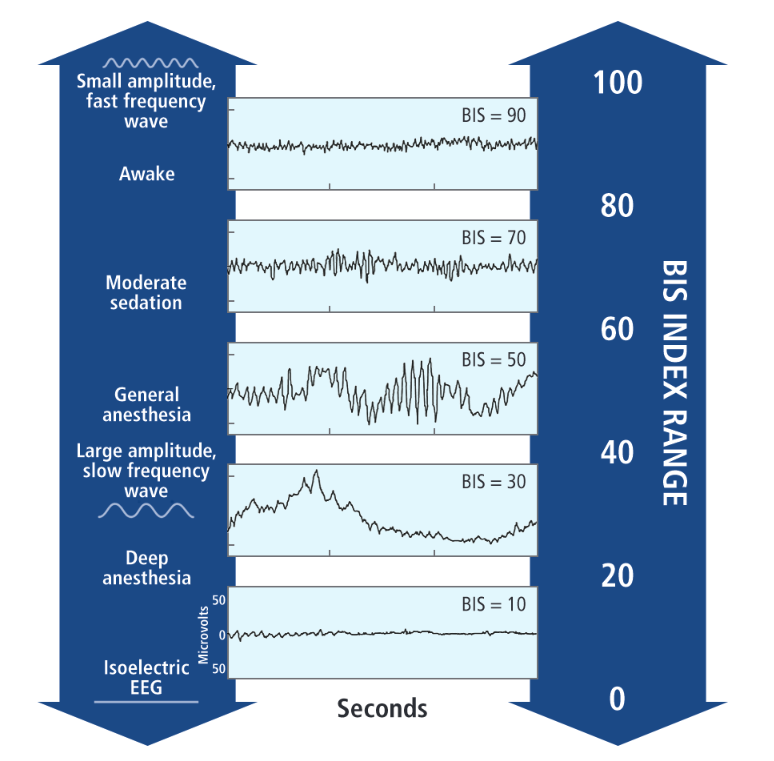 Figure 2. BIS index is scaled to correlate with important clinical end points during the administration of Propofol
Figure 2. BIS index is scaled to correlate with important clinical end points during the administration of Propofol
The control of BIS number is critical to the Propofol delivery process as it represents the behavior of central nervous system directly. However, the BIS monitoring can be significantly influenced as an indicator of anesthetic hypnotic effect during the operation. Four key areas include the influence of muscle tone (EMG) from the forehead muscles; electrical and mechanical artifacts from medical devices; abnormal EEG states; and certain anesthetic agents and adjuvants—which can all lead to elevated BIS values. As a result, ideally BIS monitoring information should be integrated with other available monitoring information and patient assessment, such as blood pressure and heart rate etc.
Unintended intraoperative awareness may occur in 0.1% to 0.2% of adult patients undergoing general anesthesia. Inadequate anesthetic effect results from an insufficient anesthetic dose, disruption of anesthetic delivery, or potentially inherent anesthetic resistance. Because of the potential for psychological injury, clinicians should consider this evidence in developing patient-specific strategies in order to avoid awareness.
The use of an automated closed-loop controlled Propofol delivery system using BIS monitoring reduces primary anesthetic use as well as emergence and recovery time. Experiment that utilized Propofol reveals that 13% to 23% less hypnotic drug was used and 35% to 40% quicker wake up was obtained, which significantly reduces the cost of clinic. Incidence of intraoperative awareness and recall can be decreased by strictly controlling the BIS value between 45 to 60 and avoiding value greater than 60. The evidence of the significant benefit is shown by the fact that only two patients in the 4,945 treated patients reported awareness, with a 77% reduction comparing to prior study.
What about the application needs controlling?
The manipulated variable for an automated feedback controlled propofol delivery system will be the amount of propofol injected. The amount of anesthesia injected is always the only variable that can be controlled in a closed loop drug delivery system and it makes practical sense since modern technology allows us to directly change the input amount.
There are two ways of Propofol intravenous infusion: manually controlled (MCI) where the anesthetist makes each change to the infusion rate or target-controlled (TCI) where the anesthetist sets a target blood or effect-site concentration and the computerized infusion device makes the necessary changes to the infusion rate. A TCI pump in combination with the BIS monitoring system would be the most suitable choice for Propofol intravenous infusion to control the controlled variables.
Generally, the BIS value will be set to 50 for a feedback loop. A TCI pump is used to titrate the drug delivery to the indicator of depth of anesthesia. A model-based adaptive controller will be designed to steer the feedback system. The controller will contain an algorithm to translate the difference between measured BIS value and set point to a particular action of the TCI pump.
The individual anesthetics produce specific pharmacological actions so the unifying concept of “depth of anesthesia” may need to be revised. When looking at the dataset collected in their experiment, patients without awareness had BIS value ranged from 50 to 80. As a result, it becomes necessary to operate in an individualized range.
What could happen to our system?
Potential sources of disturbance include the sudden jump of BIS value caused by the influence of muscle tone (EMG) from the forehead muscles; electrical and mechanical artifacts from medical devices; abnormal EEG states; and certain anesthetic agents and adjuvants. These unmeasurable disturbances which are not considered in the controller synthesis urge the presence of an anesthesiologist to counteract them.
A feedback system will be appropriate for the Propofol delivery due to the characteristics of the TCI pump. Feedback system represents a situation in which two (or more) dynamical systems are connected together in such that each system influences the other and their dynamics are thus strongly coupled. A feedback system is a common and powerful tool when designing a control system. Basic components of a feedback control system are the control variable, the set point for this variable, which is the chosen target value specified by the user and the controller to control the actuator. Propofol delivery feedback system contains a sensor that monitors the BIS value, a controller that compares the measured value to the set point and sends the decision to the actuator-pump which has an effect on different body functions. The TCI pump reacts accordingly by increasing or decreasing the amount of input, which is the amount of Propofol infusion. Success of feedback controllers for anesthesia largely depends on the sensors that measure the different components of anesthesia.
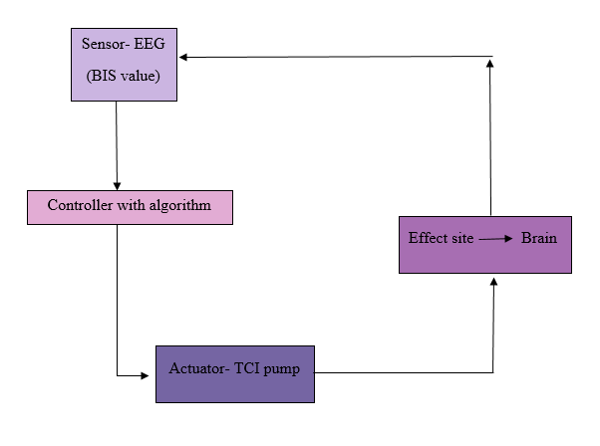 Figure 3. Broad framework of closed-loop Propofol delivery system
Figure 3. Broad framework of closed-loop Propofol delivery system
A closed-loop system senses the level of output, feedbacks this information, compares it to a set point that defines the desired output level and uses the difference to push the output towards the set point. Because of more frequent sampling of the control variable and more frequent changes to the rate of drug delivery than with manually delivered anaesthesia, the stability of the control variable may be greater. At the same time, the dose delivered is customized to meet the exact requirements of each patient, thereby overcoming the problems of inter-individual differences and differing levels of surgical stimulation.
Citations:
Ngai Liu, M.D.; Thierry Chazot, M.D.; Antoine Genty, M.D, “Titration of Propofol for Anesthetic Induction and Maintenance Guided by the Bispectral Index: Closed-loop versus Manual Control: A Prospective, Randomized, and Multicenter Study” Clinical Science, April 2006, Anesthesiology 4 2006, Vol.104, 686-695.
Mortier E1, Struys M, De Smet T, Versichelen L, Rolly G, “Closed-loop controlled administration of propofol using bispectral analysis” , Anaesthesia, 1998, 53, pages 749-754
D.Kelly,Scott, MD “Monitoring Consciousness Using the Bispectral Index (BIS) During Anesthesia” Monitoring Conciousness
Leslie K1, Clavisi O, Hargrove J. “Target-controlled infusion versus manually-controlled infusion of propofol for general anaesthesia or sedation in adults” Cochrane Anaesthesia Group, 2008, DOI:10.1002/14651858.CD006059.pub2
C.Frankel Todd, “We are convinced the machine can do better than human anesthesiologista”, May 15, 2015, The Washington Post
Peter S. A. Glass, M.B., Ch.B., F.F.A.(S.A.), Professor and Chairman; Ira J. Rampil, M.S.E.E., M.D., Professor of Anesthesiol- ogy, “ Automated Anesthesia: Fact or Fantasy?” , Anesthesiology 7 2001, Vol.95, 1-2.
D. Puri.G, “Closed Loop Anaesthesia Delivery System (CLADS)- Anaesthesia Robot”, Institute of Medical Education and Research, Chandigarh, 160012, India
Figure 2 explaining the BIS index was very necessary and came at the correct time in the article. I appreciated the informational graphic as it made it easier to understand the complex idea.
The evidence from the study helped to substantiate the importance of the application. I was not aware of the problems occurring within the anesthetic world, but I can agree that anything that helps with being knocked out during a difficult procedure is a very important topic to look into. Reducing the cost to the clinic and workload of the anesthesiologist is important as it could also lower the cost of the procedure if it reduces the complexity in the long run which is also important to the medical field.
It is important that the controlled and manipulated variables are stated clearly for this process as it is a bit more difficult of an idea to work with and allows the reader to ground exactly what is happening in the system with these specifications.
The potential disturbance variables include sudden jumps in readings. As we recently went some different controller schemes, it might be interesting to propose which type of controller scheme would aid in reducing the effects of the different disturbance variables on the output of the system. Figure 3 was useful in understanding the general outline of the control loop proposed.
At the end of the article, the authors return to the reason why their product is important and how it will better the current procedure, which is important in reminding the reader why everything that was said so far mattered.
I think this article has great technical content, but is not super reader friendly. This reads a bit more like a research article than a blog post. A bit more relaxed language would help with the readability. Another suggestion would be breaking up the article more into smaller almost question and answer sections so that the reader can follow exactly what is being explained as the post goes along. This is a higher level application that requires a bit more scientific and specific language, and could be helped further explanation as to what certain things are and why they are important on a lower level.
This blog post was written very well and has all of the correct content. It is also very intriguing and definitely has a current market. I think the proposed control scheme makes sense and the disturbance variables are clearly listed. While they were addressed by saying that an anesthesiologist would still need to be present, it would be interesting if there were any other potential ideas for controlling these disturbance variables or reacting to them.
I enjoyed reading this article and feel like I learned something new and very important. I hope I have one of these machines helping my anesthesiologist if I get surgery!
This entire article was incredibly interesting to read! I was shocked by how close it seems we may be to offering robotic, physician care. Personally, I cannot help but be a little nervous to let a machine administer a drug to patients that has fatal side effects when taken in too large of a dose. Nevertheless, if the system is proven to be more precise in its administration than current techniques, then I can see this being implemented into health care in the near future.
This being said, I think a little more depth into how exactly the system would work in a health care environment would be useful. For example, are human anthologists still needed to operate the machinery or can the set point just be determined by some computer algorithm and then any individual in the hospital can set the machine to that set-point and hook it up to the patient? If the use of a trained human is still required then I think it would be interesting to ponder the usefulness of this system, economically. Right now, anesthesiologists are paid large salaries to complete their job, in part because of the many years of training it takes to master this skill. That being said, if they are still needed as more of a back-up measure if the system were to fail, would they still be paid the same or would their salary decrease. I am aware this is something that you may not know, but it is definitely interesting to think about, because if both the machine and anesthesiologist cost a lot of money to the hospital, then what would be the advantage of having/ using both when the human anesthesiologist produces similar, albeit less precise, results.
On another note, all parts of the proposed scheme were extremely well explained. At no point did I find myself questioning any of the medical terminology used throughout the article. I also thought that all of the figures used were extremely helpful in discussing your topics and helping the reader to visualize the processes you were speaking of. This especially holds true for the BIS index in figure 2, since that is an obscure topic when you first hear about it. In general, the feed-back loop proposed is by far the best, and likely only option in this application, seeing as disturbances may come from many different avenues in the body/ physiology of the patient and as such the system should be equipped to handle all of these potential disturbances appropriately.
Again, this article was extremely well thought out and kept my attention the whole time! I am interested to see where this may take the world of medicine in the years to come! Nice job!
First of all, I think you guys did a really good job! Thanks for your guys’ project, I learned something I never touched before. I believe this technology will definitely benefit patients in surgeries.
The structure of this paper is well organized. It first introduces the background information of this technique and then states how it works. The proposed control scheme is well explained and reasonable. I really like figures you provided in the paper since it did help me understand those subtle and unfamiliar terms such as the BIS index. The proposed control scheme is well explained and reasonable. As you guys said in the paper, the controlled variables include the measurement of the heart rate, blood pressure, respiration and oxygen level in the blood. Because of these variables varied significantly for people with different age, gender and other factors, EEG and BIS are chosen as the alternatives. In this system, the amount of propofol injected is the manipulated variable. The potential disturbances for this system include the sudden jumps in reading of the BIS. I think your manipulated and controlled variables are able to meet your expectation that delivery of propofol can be performed automatically and reducing the cost to the clinic as well as the workload of the anesthesiologist. To alleviate the effect brought from the disturbance, sudden jumps of the BIS, I think it is possible to add a PID controller into your loop as the PID controller is able to adjust the error will happen.
Reading this article does make me learn something new but I have to say it is not easy to read as I spent more time on reading and understanding the information provided in this article than I did in another one. I think the form and content of this article are more like a research paper instead of a blog. I think it is better to separate this article into several small pieces and just introduce one piece completely. It might be helpful for people who do not have enough background information on drug delivery to read and understand.
Although I do think your designs are applicable, there is one major aspect is necessary for you guys to investigate – the cost. It is necessary to compare the cost of traditional propofol delivery with the automatic one. If the cost of the automatic one is pretty high, it might not be an appropriate application in the future surgeries for patients. In addition, in the article, with the help of this new system, an anesthesiologist would still need to be present. As a result, this automatic drug delivery system does not totally replace the role as the anesthesiologist does. In this way, it is hard to decrease the clinic cost and make people willing to adopt this technique.
I really enjoy reading this article and believe with the progress of biomolecular engineering, this automated closed-loop controlled propofol delivery system will definitely be the reality.
As an avid Grey’s Anatomy fan, I consider myself to be well-versed with the happenings in ORs, yet no amount of binge watching Grey’s on Netflix could prepare me for this groundbreaking research on a propofol delivery system. The idea behind this closed-loop propofol delivery system and its potential implications on the health care system are truly amazing.
Despite being a very complex topic, I think the functionality of this propofol delivery system was explained well given the target audience. The schematic highlighting the feedback loop that would be implemented in this control scheme was a nice touch to enhance the clarity of the system. From this schematic, it can be gleaned that propofol injections will be manipulated based upon BIS measurements. The control variable BIS is multifaceted and not an inherently tangible topic for most readers, but I think the correct level of detail was included to provide readers with a basic understanding of BIS’s effect on anesthesia. Although I do have some background in biochemistry and human anatomy, I think that the information contained in this article is accessible to the average reader.
I think the proposed controlled scheme would be very effective in controlling BIS in patients undergoing surgery. Potential disturbance variables that would cause a sudden jump in the BIS value were also appropriately addressed. Although not considered in the controller synthesis, they highlight the need for a technician during all procedures. I think another potential disturbance variable may be electrical issues with the sensor and/or actuator. Hospitals are well equipped with various back-up energy sources but unexpected malfunctions happen. When something as valuable as a person’s life is on the line, I think that it would be almost necessary to have an anesthesiologist present during all procedures to ensure that the control scheme is functioning properly.
As sad as it may be, the American health care system, like any other profitable business, is obsessed with money. Anesthesia drugs, like propofol, and anesthesiologists are expensive. Therefore, I think the health care system will quickly utilize this closed-loop propofol delivery system since this control scheme allows for a more precise amount of propofol to be administered, eliminating the waste of expensive drugs. I am not sure if the general public will be as excited about an automated anesthetic machine, however. Surgeries are often surrounded by clouds of intense emotions as the patient and their close friends and family attempt to do anything possible to increase the health of the individual. With this in mind, it is very understandable to see why some people may be skeptical of allowing the consciousness of their loved one be dictated by a machine. When you think about it, however, some of the most effective medical advances were initially received with skepticism. For example, I recently read an article about the invention of incubators. Despite the fact they are now used ubiquitously in hospitals for newborn babies, the public was originally not very accepting of this technology. Only time and consistent results can sway public opinion on such a topic. I think the results of more studies and clinical trials will need to be shared with the public in order to convince everyone of this control scheme’s amazing potential impact.
It was very exciting to learn about this new medical advancement. Welcome to the future, everyone.
This article is very informative about how anesthesia works and how to measure if the patients are completely under or they still have conciseness with the anesthesia. It is also a very interesting idea since that deliver propofol automative instead of manually since that manual injection might not be as accurate and efficient as automative because there can be a lot more errors happen to the patient when it is manual injection than automative because machine can be more precise than human can be. Therefore, this application makes sense that it wants to make the propofol injection system automative so reduce error, since anesthesia process is a very delicate process.
The control scheme is pretty clear and makes sense. The manipulated variable is the amount of propofol injected and the control variable is the state of conciseness of the patient, and the state of conciseness is being measured by BIS value, which can be deduced by the four different measurements you guys mentioned above. For the disturbance variable, I think that since the control loop is measuring the BIS values, so the sudden jump of BIS values from the patient might cause danger since the control system might accidentally inject more propofol into the system when it is not needed. That can cause danger to the patient’s health and also it will be a waste of the anesthesia. I think it should set an algorithm that if the patient’s BIS value increase to a certain level, then inject more propofol and not just making adjustments for a slight deviation.
Overall, I think it is a good idea to have an automative, controlled propofol delivery system since it can mean a safer way to deliver anesthesia than by a doctor because human generally makes more errors than the machine, and an over or under dose of the propofol will result in the discomfort of the patient either during or after the operation. So a closely measure and controlled anesthesia deliver system would be a very helpful thing to have. The problem about the automative systems is that the set point can be changed by someone either intentionally or unintentionally, which can cause various issues. So even though it is automative system, the doctor should check on the system before and during the operation. People might not like the idea of a machine doing all the work either because they are anesthesiologist and they are being replaced by the machine or some people just do not really like the idea of machine doing people’s work or they are afraid of machines. But the time will ease the problem just like what happen during the industry revolution when machine starts to do the work of man.
Overall, this is a very interesting read and a very informative too. Great job.