Whether you are a sugar daddy or monitoring your sugar levels, you are just trying to stay in control of your life, whether that be diabetes or otherwise. When food is consumed, the body breaks down the sugars and starches into a simple sugar commonly referred to as glucose. Glucose, which is stored in the bloodstream, is used by the body as a form of energy. Like every consumer product in a Giants food store aisle, diabetes too comes in different types. In Type 1, often known as juvenile diabetes, the pancreas in your body do not produce insulin. Instead the body’s immune system attacks and destroys the beta cells that produce insulin in the body. Alternately, in Type 2 diabetes, your body becomes resistant to insulin. To dia ‘beat’ this resistance, your pancreas makes extra insulin, but over time your body may be unable to make enough insulin, resulting in Type 2 diabetes. Diabetics suffer from major health complications and other daily side effects with symptoms including dehydration, frequent urination, increased appetite, high blood pressure, and damaged blood vessels. These side effects are dia-… we’re out of puns for now.
The not-so sugar coated fact is that 1.25 million Americans are living with Type 1 diabetes. This breaks down to about 200,000 youth and over a million adults who are currently suffering from diabetes. This sugar high isn’t stopping anytime soon, it is projected that by 2050, about 5 million people in the U.S alone will suffer from diabetes, including nearly 600,000 adolescents. Not so sweet, eh?
Diabetes was the seventh leading cause of death in the United States in 2010 based on the 69,071 death certificates in which diabetes was listed as the underlying cause of death. In 2010, diabetes was mentioned as a cause of death in a total of 234,051 certificates.
Diabetes may be underreported as a cause of death. Studies have found that only about 35% to 40% of people with diabetes who died had diabetes listed anywhere on the death certificate and about 10% to 15% had it listed as the underlying cause of death.
Apart from the overwhelming death numbers, diabetes comes with a high cost, literally. In the early 2000’s, insulin cost nearly $100-$200 a month, but now has peaked to about $400 – $500 a month. That’s a whopping $4800-$6000 a year for a painfully pricking process. Neither one’s sugar level nor the price of insulin, should be that high. In addition to the diabetic bills, the increased risks of anxiety and depression for people, especially children, with diabetes pricks your heart deeper than a needle could ever prick a finger. Not so finger pricking good?
One of the best ways to take control over this alarming sugar rush is by the constant monitoring of one’s blood glucose levels. Glucose levels fluctuate throughout the day based on a person’s diet, activity levels, and other external factors. As such, it is required that one’s blood glucose levels are obtained before and/or after each meal. Today, the most widely used glucose monitoring devices are based on minimally-invasive finger stick tests, a market that is worth over $6.0 billion. This process leaves patients having to frequently prick their skin, for some, upwards of six times a day! As such, the introduction of both non-invasive glucose monitors (NGM) as well as continuous glucose monitoring systems (CGMS) is of great interest for diabetics and healthcare professionals alike. Today, NGM options on are the market are mainly subcutaneous sensors. These types of are NGMs are associated with painful, subcutaneous implants that require replacement within a matter of days, in addition to unreasonably high user costs. Yet, with scientific and technological advances and knowledge higher than before…why are diabetics stuck suffering? Our process aims to eliminate this painfully, invasive process and take the “ouch” out of the day-to-day life for millions of people.
Our goal is to cut out all of the pain associated with a diabetic diagnosis. This is possible thanks to state-of-the-art technologies, which take advantage of optical glucose monitoring as well as previously established methods of CGMS and insulin pumps. In particular, our control scheme functions by using non-invasive contact lenses as our sensor to measure glucose levels. The reading is then translated into a signal which can be interpreted by a proportional-integral-derivative (PID) controller, which continuously calculates the error between a patient’s current and optimal glucose levels. This is done by analyzing the difference between the desired set point and the actual value of the blood glucose. The desired set point will be personalized based on demographic factors like age, gender and other health conditions. The PID controller will interpret the signal and output a specific, continual insulin response via an insulin pump. Readings will be stored and displayed via the CGMS. The advantages of implementing CGMS to applications are of immense need within the diabetic community. These continual readings will allow healthcare professionals with useful information about trends in a patient’s daily glucose levels, helping patients to reduce glycemic variability. This additional control will aid in the prevention of hypoglycemic episodes and lower glucose levels.
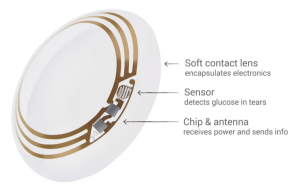
The proposed contact lenses work according to the image above. There is a clear layer, much like that of a regular contact lens that surrounds most of the electronics. Connected to these electronics is a sensor that can measure the glucose concentration in the tears of a patient. This information, via the encapsulated electronics, would wirelessly be sent to a device which would determine whether the glucose level is in the appropriate range. From this, the device would determine whether to inject insulin or not when appropriate.
In particular, the process aims to gain control of glucose levels, insulin must be injected on an as-needed basis into the patient. For this to occur, the amount of insulin injected at variously points within the day must be altered according to the unique “healthy” glucose ranges 4–8 mM (72–144 mg/dL)of each individual. There is potential to also control the times at which glucose levels are measured, but it is more advantageous for levels for be read and recorded on a near continuous basis. Continuous readings would also allow for a more complete picture of the fluctuations in glucose levels throughout the day.
This process is cyclical in nature, but ultimately works to create a connection between glucose readings and impart an appropriate insulin injection response. As such, it is crucial that our device is continuously functioning at its highest capacity, and although the functionality of our device is ultimately aimed to increased ease and quality of life for the user, the process itself is delivering life-sustaining hormones to the body, and thus much be extremely efficient and precise.
Although this idea is melt-in-your-mouth good, some logistical issues arise from the combination of contact lenses and insulin injections. For instance, the contact lenses are not permanent; over time they will degrade and readings will become less accurate. A study would need to be done on the optimal lifetime of a set of lenses would last. Supposing proper functionality of the device, the device would need to be able to determine the minimum blood-glucose level a patient could have and inject insulin when below this threshold.

An additional issue with these lenses is manufacturing, and ultimately cost to consumers. Not only is the purchase of insulin expensive, but also, some of the prototypes of these devices use partially gold wiring within the contact lens. Despite looking cool, the cost of a set of contact lenses would be even higher than that of insulin. Google is still in the testing phase of these kinds of contact lenses, therefore there is no cost that has been quoted for use, but would very likely be expensive given the manufacturing cost and the luxury of use. There are those who believe that competition among manufacturers will drive down the cost of glucose reading lenses. Others believe that if the price does not get driven down by competition that insurance would most likely cover these devices.
The system that we have described is known as a feedback loop. A feedback loop is a control system that responds to a perturbation after it occurs. This is opposed to what is known as a feed-forward control system. A feed-forward control system is one that measures a change in input and adjusts before a change in output occurs. In our case, a human body would need a measurement to be made of system “inputs” or what a given person eats. If a response were to be made before moving above or below critical blood glucose levels, it would be invasive to the point that one would have to have a device implanted in their stomach to determine “system” inputs. This kind of implant is impractical and would not be a product worth selling. Responding after a change in blood glucose better treats those with Type 1 and Type 2 diabetes by its less invasive style and its improvement on the current finger pricking pain that regular patients go through.
At the end of the date, our process is the sweetest proposal for controlling diabetes in a pain free manner all while offering extensive sight into a patient’s daily glucose trends. Both of which would make the projected increase in diabetic diagnoses in the future a little easier to swallow.
References:
“Continuous Glucose Monitoring.” Dexcom. Dexcom, 26 Jan. 2017. Web. 10 Mar. 2017.
Sawh, Michael. “Triggerfish Smart Contact Lens All Set to Tackle Glaucoma.” Wareable. Wareable, 08 Mar. 2016. Web. 8 Mar. 2017.
“SENSIMED Triggerfish®.” SENSIMED Triggerfish® – Sensimed. Sensimed, n.d. Web. 10 Mar. 2017.
Shah, Rima B. et al. “Insulin Delivery Methods: Past, Present and Future.” International Journal of Pharmaceutical Investigation 6.1 (2016): 1–9. PMC. Web. 30 Mar. 2017.
“Type 1 Diabetes Facts.” JDRF. N.p., n.d. Web. 10 Mar. 2017.
Vashist SK. Continuous Glucose Monitoring Systems: A Review. Diagnostics. 2013; 3(4):385-412.
First off, I really enjoyed all of the puns. It definitely kept your article easy and fun to read! Contact lenses as a diagnostic for glucose levels in diabetics is a wonderful idea, and it definitely makes sense to avoid checking levels through painful pricking using needles. I think that this is such a useful product and would be marketable to a large audience. You did a very nice job explaining how Diabetes affects so many people and that it is projected to affect even more in the future. Therefore, the market is very large for your idea. Not only will it reduce the pain experienced through checking levels, but it could even help save lives. I personally am very afraid of needles and could not imagine having to prick my finger multiple times in a day. I am sure there are many people with the same fear, so I think that this application would be so useful to be able to avoid that pain. In addition, because this is a continuous glucose monitoring system, a pump will release insulin if levels are too low. Therefore, the patient will not even have to think about checking their levels because the feedback loop will be attached to the pump and automatically release insulin when necessary.
This application would work with a feedback loop. I think that to improve this article you could be more specific in listing what the controlled, manipulated, and disturbance variables are. The glucose levels would be the controlled variable that would be compared to the set point. Is there a difference in the glucose levels determined by tears as opposed to the glucose levels determined in the blood? Once the contact sensors determine if the levels are too low, how much insulin must be released and what is the time frame in which it takes to get to the desired set point after releasing insulin? Would you ever run into the problem of having insulin levels that are too high and how would you account for that? Another thing to keep in mind would be if there are other disturbances and how to account for those. For example, would getting something in your eye cause the sensor to miscalculate the glucose levels and release insulin when it is not necessary?
I think that this product is potentially useful in actual practice. The cost, as you described, might outprice what is in place now depending on the lifetime of the lenses. Even if they cost more than traditional diagnostics, however, they still could be accepted by diabetics since they will eliminate the pain of the finger prick and will be easier to monitor. More studies would need to be done on the accuracy of this method at determining glucose levels. The manufacturing of the contacts might also have some limitations as you described. I also think that this device would be so useful because the continuous data could be attained over time for a patient which would give insight into the fluctuations of levels glucose over the course of a day. I think you all did a great job and that this might be the future for diabetics!
Before I start, I appreciated all the puns a lot. As someone who loves puns, it kept me paying attention to the detail of the article and therefore helped me read about the important aspects of the device much more closely. From an application standpoint, I think this is an incredibly useful device that as technology becomes more developed could become a realistic treatment device for diabetes. Since I do not have diabetes I can’t see myself using the device, however, knowing from friends with diabetes the inconvenience of today’s treatments, it would be a device that I could see those who need the treatment using. Along with this, you state how companies are already working on similar devices and thus this is a very realistic medical device of the near future.
The scheme of this device makes a lot of sense for how it would work. The article does a great job of pointing out that glucose level will be controlled to a persons’ normal range by injecting insulin through an insulin pump after a sensor in a contact lens reads a fluctuation in the user’s glucose level. Although there is no mention of disturbances that would affect the reading of the sensor, there is plenty of mention of the logistical errors that could cause the contacts to fail. The failure of the contact lenses would be a result of two errors. First, the life of the contact is not known so the degradation could cause the lens to no longer work. Second, you mention that the lenses would be very expensive and therefore not readily available for all who need it. I liked that these two problems were mentioned because I was thinking of these issues, as well as the possibility of insurance companies paying for the lenses, prior to reaching those points in the article. All in all, I found that you did a good job of describing the variables of the process.
In the end, I find that once enough information is known about the pricing and the life of the lenses, it will be a very useful device for those who are suffering from diabetes. I find that you touched up on all of the concerns that I would have had with the feasibility of the device. For the sake of people with diabetes, I hope that this device does in fact get produced. Aside from the fact that not enough information is known on the life and price of the lenses, this device and process will be very useful in the near future.
This group did a fantastic job at presenting their project idea in a very educational yet conversational tone. I stopped reading this article feeling like I had genuinely learned something new and interesting. The group presented the problems of diabetes in a very clear manner that outlined the importance and significance of the presented solution process scheme. While diabetes is a large issue that brings many obstacles to its victims, the group decided to focus on a single issue: diagnostics of glucose methods. The group presented the current level of technology that is accessible to diabetes patients in an attempt to innovate the process of glucose level monitoring, a tasking and painful trial that diabetics have no choice but to put up with. The proposed non-invasive glucose monitor is not only comfortable, but takes away the task of frequent immediate blood tests. A continuous glucose monitor that doesn’t need blood is probably one of every diabetic’s dreams.
The technology behind an optical glucose sensor is very innovative and impressive. Reading the article for the first time, I could tell what problem the group was aiming to solve, but the actual solution being a wearable contact lens that runs continuous level tests is revolutionary and honestly caught me by surprise. The image presented in the blog provides a very understandable explanation as to how the process would work, through measuring the sugar levels in tears and wirelessly transmitting the levels to an insulin pump controller, without the patient needing to actively do anything. There is definite appeal in this product and I can see it being the standard method of diabetes control in the near future.
While obviously the glucose monitoring contact lens is an amazing idea, it contains many flaws as an idea. The group did a good job at foreseeing the problems that would come with their proposed process scheme such as high costs and loss of accuracy over time/lifetime of product. There are other flaws, however, that were not readily addressed, such as the fragility of such a delicate piece of technology. Contact lenses alone are very delicate and can break or dry up quite easily. Lenses need to be maintained at certain moisture levels in order to still be wearable, however a liquid solution could be very damaging to an internal circuit and signaling system, which might not be completely protected or insulated. Another issue is comfort and cleanliness. Many people don’t like putting physical objects into their eyes, even as an alternative to finger pricks, especially if the contact lens would have to be heavier and more rigid than a basic 9non-circuited) contact lens. Contact lenses also have to be maintained at a certain level of cleanliness in order to prevent infection of and damage to the eyes. While there is a clear relief to the standard discomforts and obstacles of glucose diagnostics, it seems as though alternative comfort issues arise with this solution.
From reading this article, I have fallen in love with the idea of the contact lens glucose monitor, but I cannot help but see many potential issues that weren’t necessarily addressed by the group’s proposal article. That being said, electronic contact lenses are a technological field still undergoing much research and development, and the technology necessary for the implementation of circuitry into wearable contact lenses might have to take into account comfort, maintenance, and delicacy in its basic developments. This idea is well presented, well thought out, and definitely desirable to diabetic consumers, with the largest issues in application being high costs and the unknowns that come along with new technologies still under development, both of which were addressed by the group. Good Job!
I enjoyed reading this article since it has provided me some valuable information that I didn’t know about diabetes and the technologies for diabetic patients nowadays. The use of contact lenses as a sensor to measure glucose level. The reading obtained will be translated into a signal and interpreted by PID controller which calculate patient’s glucose level, therefore, the application makes sense. I’m sure many diabetic patients want to try this technology if it cuts out the pain associated with a diabetic diagnosis.
For this application, its main aim is to gain control of glucose level and the proposed control scheme makes sense. As mentioned in the article, the insulin must be injected as needed by the patient and the amount of insulin injected must be altered within one day. It is also important to control the times at which glucose levels are measured. The article did a great job in explaining why a feedback loop works for this application but, I couldn’t see any disturbance variables for this application in the article. My concern for this product might be how accurately blood glucose levels can be obtained using tears and does having eye disease/ irritation influence the result?
I agree with the logistical issues arise in the article about the combination of contact lenses and insulin injections. The contact lenses being degradable and the cost related to manufacturing of the lenses will make it harder for every diabetic patient to afford this technology. I believe this technology might decrease the pain related to a diabetic diagnosis for patients so, I hope there will be different ways to minimize the cost in the future.
I think this is a very creative and practical device, and could certainly help the millions of people suffering from diabetes. You clearly established that there is a large market for such a device, and that is has the potential to not only increase the comfort of patients with diabetes, but the ability to save their lives. I like the use of contacts as a minimally invasive way of monitoring glucose levels, as I can imagine that pricking your finger on a regular less is less than pleasant. I also like that it monitors glucose levels on a continuous basis rather than just at specific intervals. I think this eliminates some of the dangers that come with unexpected changes in glucose levels, as the system is able to take the appropriate action before the situation becomes life threatening. One concern for the device is whether it will accurately be able to monitor glucose levels through the tears of patients. You mentioned that glucose is stored in the blood, so will the concentration of glucose in the tears be the same of that in the blood? If this is not the case, having the sensor measure glucose levels in the tears and producing a response based off of this could potentially be very dangerous for the patient. Also, I wasn’t clear on how the insulin would be injected into the body. Would it come directly from the contact lenses, or would there be a separate device the injected it directly into the blood stream? Something to consider with this is how long it will take for the insulin to be transported throughout the body because it does not occur rapidly there could be damaging health effects for the patient.
Your control scheme makes sense and is easy to understand. Given that the main problem for diabetics is glucose levels, it makes sense that you chose that to be the control variable you are monitoring. Having insulin be the manipulated variable also makes sense as that is how diabetics control their glucose level. You don’t explicitly mention it, but I would assume disturbance variables include food intake, exercise, and other things that affect glucose levels. I think this process does have the ability to control and account for disturbances and variations in glucose levels. I think this product could potentially be viable on the market, but some concerns would need to be addressed. The largest concern, which you mentioned, is the cost of the lenses. At least at the early stages, they are bound to be very expensive, and there is no guarantee that enough people will be able to afford them to create a market. Additionally, insurance companies might favor the less expensive glucose measuring methods, rather than covering this new, expensive method. Finally, research would also need to be done to ensure that the contacts will not do any permanent damage to the eye. Overall, I think this is a very clever idea that with some work could help millions of diabetics.
As an initial observation, I really enjoyed the reading this post due to its quality organization and inclusion of humor. The use of puns was stand-out and kept me engaged throughout the first few paragraphs, but fell off towards the end. I would have loved to see a continuation of the humor throughout the entire post. That said, I thought the way the post was organized as a whole was outstanding. The issue was established well and the need for a new technology was demonstrated early on, before moving on the fundamental idea and finally the logistics, such as cost and long term viability.
This application is novel and creative, and I can envision it being used to treat diabetes in the near future. It is not made clear whether or not optical glucose measurement is a currently available technology, so I am unsure just how far off this idea could be from reality. However, assuming that glucose can be measured through the eye, I could see this technology replacing more invasive blood testing norms. This is a more non-invasive technique, but contact lenses are still fairly intrusive. Would there be a measurement method that would have less invasive means? Also, the system requires an insulin pump be used, which is also a major ordeal.
The control scheme being utilized absolutely makes sense. The use of feedback control is appropriate, when compared to the alternative of a feed forward system. The identification of a set point and reference to deviation from that set point are good details. It is unclear, however, as to how the insulin injection will be managed. Would the goal be an underdamped response? This would lead to fluctuating glucose levels, which could not be good for the diabetic subject. Or would you opt for an over damped response? This could result in a slow response time, leading to unnecessary discomfort for a longer period of time.
I believe that this application would be highly useful for anyone suffering from diabetes and, given a few breakthroughs, could be used within the near future. The limiting factor, I believe, will be the cost of the lenses, especially because they will need to be replaceable. As such, manufacturing costs will need to be reduced tremendously, especially since this technology is still in very early stages of development. That said, I think that if cost is kept low enough, this could be a system used by every diabetic in the world. I appreciate the thought put into the post, and I like the idea very much. Great work!