Because Dr. Koplin is an ophthalmologist by trade, it is only natural that he uses the eye and cataracts (his particular area of expertise) as a model of innovation. He does an excellent job of thoroughly explaining much of the necessary anatomy and technology involved in operating on cataracts in his talk. Here is some of the most important information regarding the anatomy of the eye and cataract surgical technique today, as well as a description of Dr. Koplin’s own innovation in topographical mapping of the cornea.
Anatomy of the Eye
The eye is one of the smallest and most complex organs in the body and is generally compared to a digital camera in how it functions. Light is primarily focused by the cornea, the clear front surface of the eye (like a camera lens). The iris controls the amount of light that reaches the back of the eye by controlling the aperture of the pupil, much like a camera’s diaphragm. The lens located behind the pupil further focuses light, automatically focusing on objects at different distances (think autofocus camera lens). Finally, light reaches the back of the eye where it is converted to electronic signals like the electronic image sensor of a digital camera. The retina (this light-sensitive surface) is connected to the optic nerve, which transmits the electronic signals to the visual cortex of the brain, the region that controls sight.
 The most important structures of the eye for our purpose of understanding cataracts are the cornea, anterior chamber, pupil, lens, and suspensory ligaments (also called zonules).
The most important structures of the eye for our purpose of understanding cataracts are the cornea, anterior chamber, pupil, lens, and suspensory ligaments (also called zonules).
Cataract Surgical Technique and Technology
A cataracts is the clouding of the eye’s natural lens, usually associated with aging or certain medical conditions, like diabetes. The lens is composed of water and protein carefully ordered to allow light to pass through clearly. As the eye ages, the protein may start to clump together, clouding vision. Cataracts that severely impair vision can only be corrected surgically.
In order to have a secure operation, there are a number of items necessary.
Sutures: Sutures are absorbable or non-absorbable synthetic polymers used to close open wounds and can exist as a single filament or, more often, as many filaments braided together. Suture structure and composition varies based on the intended use. For cataract surgery, sutures are as small as 0.02mm in diameter…half the thickness of a hair! These minuscule sutures have been made possible by recent advancements in polymer extrusion methods, the process by which polymers are separated into the filaments braided to form sutures.
Microscopes: Vast improvements in microscopes and optic technology allow the surgeon to actually see what he is doing while performing microsurgery.
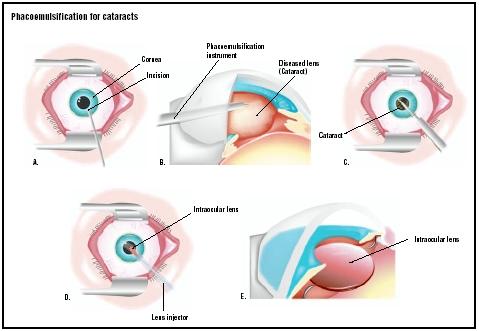
Ultrasound: Cavitron invented the first ultrasonic cataract removal device. Similar to the handheld tool used to remove plaque from teeth at the dentist, this device uses high speed sound waves to break up the lens. In surgery, this device is inserted through a small opening in the cornea and effectively emulsifies the lens. This allows the liquified lens to be aspirated from the eye. This type of cataract surgery is known as phacoemulsification. The aspirated fluids are are replaced with a balanced saline solution (this mimics the natural salt content of the eye). The replacement solution also serves to maintain the integrity of the anterior chamber of the eye and to cool the ultrasonic hand piece.
Intraocular Lenses: During World War II, Harold Ridley, a Royal Air Force eye surgeon discovered that eyes did not negatively respond to imbedded plastic. This led to the development of plastic replacement lenses for cataract patients. When implanted in the anterior chamber, these lenses restore vision to a natural state. Intraocular lenses are an excellent alternative to troublesome contact lenses or the glasses needed to correct for aphakia (absence of a lens), which caused a debilitating distortion of vision.
Corneal Topography
This is a non-invasive medical imaging technique is used to map the surface of the cornea, providing information crucial in determining visual acuity and corneal health. This 3-D map is especially helpful in planning cataract surgery and aids in placement of the intraocular lens. Dr. Koplin began his work with this technology; however, the computational power needed to support his innovative model for a digitalized 3-D map of the corneal was not yet available. In the 1980s, the process of capturing a digital image and transferring it to a computer system for analysis became automatized. Dr. Koplin worked with a group of surgeons at the New York Eye and Ear Infirmary to develop and release the first fully-automated Corneal Modeling System. Initially very expensive, the prices of these systems have fallen dramatically, increasing their availability to physicians in smaller clinics.
Leave a Reply